 Feline Tooth Resorption (FTR) is a disease of the teeth and periodontium of cats. Feline Odontoclastic Resorptive Lesion (FORL) is the term used to describe the lesions present. The terms “cervical line lesions” and “neck lesions” are no longer considered appropriate for this disease. FTR represents the most common dental disease in cats presented to veterinary dentists in the United States. Various studies show the prevalence rate to be between 20 to 75%. In reality, about 50% of the feline patients presented to the veterinarian are affected by FORLs. Although there is archival evidence of FTR being around since the 13th century, there has been a marked increase in prevalence since 1970. To date, there is no proven etiology, however, association with domestication is apparent and commercial diets containing excessive vitamin D may be a possible cause. It is rare to find FTR in feral or wild felines.
Feline Tooth Resorption (FTR) is a disease of the teeth and periodontium of cats. Feline Odontoclastic Resorptive Lesion (FORL) is the term used to describe the lesions present. The terms “cervical line lesions” and “neck lesions” are no longer considered appropriate for this disease. FTR represents the most common dental disease in cats presented to veterinary dentists in the United States. Various studies show the prevalence rate to be between 20 to 75%. In reality, about 50% of the feline patients presented to the veterinarian are affected by FORLs. Although there is archival evidence of FTR being around since the 13th century, there has been a marked increase in prevalence since 1970. To date, there is no proven etiology, however, association with domestication is apparent and commercial diets containing excessive vitamin D may be a possible cause. It is rare to find FTR in feral or wild felines.
 FTR begins when odontoclasts located within the periodontal ligament begin a pathological resorption of root surface cementum, which then extends into the underlying dentin. In most cases, the process is eventually exposed to the oral cavity. There are two distinct histological types of root surface resorption: Type I (inflammatory) and Type II (replacement by bone). Type I resorption seems to be initiated by periodontal inflammation.
FTR begins when odontoclasts located within the periodontal ligament begin a pathological resorption of root surface cementum, which then extends into the underlying dentin. In most cases, the process is eventually exposed to the oral cavity. There are two distinct histological types of root surface resorption: Type I (inflammatory) and Type II (replacement by bone). Type I resorption seems to be initiated by periodontal inflammation.
FORLs are commonly discovered incidentally on oral examination. Despite the associated discomfort, most effected cats show no obvious clinical signs. Those patients that do demonstrate signs, may not do so until serious complications have occurred. Anecdotally, cats with FORLs affecting the mandibular canine teeth seem to be most likely to exhibit behavioral changes that are noticed by the owner. Clinical signs may include decreased appetite, drooling, pawing at the face, jaw chattering and reluctance to eat hard foods. The mandibular third premolar is the most commonly affected tooth and can be considered a “sentinel” for the disease. When one tooth is effected, there are commonly multiple teeth with problems.
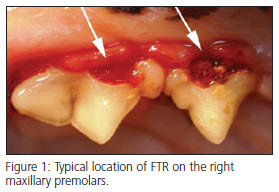
Lesions are typically found near the gingival margin on the buccal surface of the tooth, often filled with calculus or granulation tissue. They cana also be detected by palpation with a dental explorer or periodontal probe. Other common clinical findings are maxillary canine tooth extrusion (super eruption) and alveolar bone expansion (alveolar osteitis) commonly observed over the alveolar juga of the canine teeth. As with any oral disease in animals, examination is not complete until performed under general anesthesia. Full mouth intraoral (dental) radiographs are imperative for two reasons: 1) they reveal far more lesions than oral exam alone, 2) they determine therapeutic decision making.
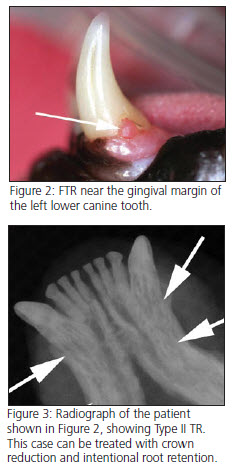
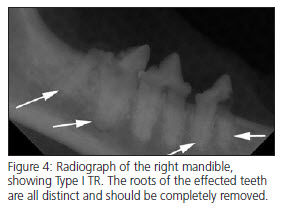 FTR may be classified as Type I (inflammatory) or Type II (replacement) based upon radiographic
FTR may be classified as Type I (inflammatory) or Type II (replacement) based upon radiographic
assessment of the alveolar bone and root. Type I lesions commonly occur in the cervical and furcational regions of the tooth. Radiographically, Type I teeth show focal loss of tooth structure and adjacent alveolar bone, with the remaining root structure being radiographically distinct from the bone. With Type II lesions the roots and the alveolar bone take on a similar radiographic appearance and cannot be easy distinguished from one another. With some multiple rooted teeth, one root may have Type I resorption, while another has Type II resorption. This combination is termed Type III resorption
Teeth with lesions exposed to the oral cavity are usually painful and secondarily infected, and complete extraction of tooth material is the treatment of choice. Teeth undergoing root resorption in the coronal half of the root will likely progress and should also be extracted. Attempts to restore TR defects have shown poor long-term success, and laser treatment is controversial. Neither of these treatment options can be recommended at this time.
Extractions are performed surgically with full thickness mucogingival flaps to allow for complete removal of tooth material, alveoloplasty, and closure of the extraction site. The use of some type of magnification greatly facilitates the procedure. Pre-op radiographs are essential for appropriate treatment planning. Type I TR requires complete removal of tooth material. Atomization (root pulverization with a high speed bur) of retained root tips should be avoided because of the potential for complications, which can include incomplete extraction, overzealous bone removal, damage to neurovascular structures, pushing root tips into the mandibular canal or nasal passages, and the incomplete resolution of clinical signs in patients with stomatitis. With early Type II cases, complete extraction is also indicated. In end-stage Type II situations, where there is advanced root replacement resorption, crown amputation with intentional root retention is an acceptable alternative. It should be noted that this technique is commonly overused in veterinary patients, resulting in painful retained roots that may never resolve. The critical factor for selecting the appropriate extraction technique is whether or not the root is radiographically distinct. The radiographic absence of a PDL, without any concurrent evidence of bony replacement of the root structure, is not an indication for the crown amputation technique. Dental radiographs commonly underestimate the presence of a periodontal ligament. Teeth with radiographically distinct roots usually have a clinical periodontal ligament and are readily extracted, in their entirety, with correct surgical extraction technique. Regardless of technique used, post-op radiographs are taken to verify removal of all dental structures.
