A middle-aged SF Golden Retriever presented for evaluation of an oral mass near on the right lower first molar (409) that had re-grown after conservative removal by the referring veterinarian. At that time no biopsy had been taken. Physical exam (Fig 1) showed a raised non-ulcerated pink firm mass approximately 6 mm in diameter located on the mesio-buccal aspect of 409. The mass was firmly attached to the underlying tissues.

Figure 1. Initial appearance of the oral mass.
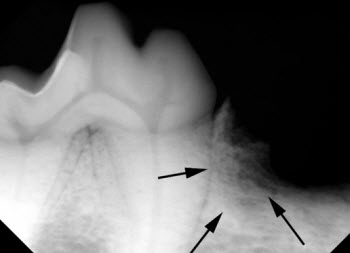
Figure 2. Dental radiograph showing bony changes associated with the mass (arrows).
The initial plan was to obtain dental radiographs of the area, biopsy the mass and conservatively de-bulk the lesion with conservative margins. The initial dental radiographs (Fig 2) showed evidence of bony invasion. After appropriate biopsy samples were obtained, the base of the lesion was de-bulked to the level of the underlying bone using a scalpel blade and electrosurgical unit (Fig 3). To avoid the potential of seeding neoplastic cells into normal tissue, no flap was raised and the site was left to heal by second intention.

Figure 3. After biopsy and conservative de-bulking of the tumor. The dark material is a hemostatic agent used to control hemorrhage.
The biopsy showed the mass to be the ossifying variant of a Peripheral Odontogenic Fibroma (POF), formerly know as an Ossifying Epulis. The epulides are benign tumors arising from developmental cells that remain in the periodontal ligament. Appropriate treatment depends on the variant of Epulis being treated. Because dental radiographs showed that the tumor had already invaded bone, the owner was given a guarded prognosis and advised to watch the area very closely for any sign of re-growth.
The patient presented 60 days later for re-evaluation of the site. The tumor had recurred in the same location (Fig 4) and was larger than when initially evaluated. Recommended margins for removal of ossifying POF’s are 0.5-1.0 cm. It was apparent that this tumor could be removed with a “rim excision” of the mandible, which would maintain the integrity of the ventral mandible. Unfortunately, achieving the appropriate margins would result in removal of most of the mesial root of 409. The owner was given the option of either extracting the distal half of 409 or maintaining most of the function of the tooth by preserving the remaining crown with root canal therapy and composite restorations. The owner elected the latter option.

Figure 4. Appearance of the mass 60 days after initial presentation
The tumor was removed en-bloc with appropriate margins, the remaining portion of the mesial root was extracted and a synthetic bone graft material (Synergy from Veterinary Transplant Services) was placed into the alveolus of the mesial root. The remaining portion of 409 was treated with root canal therapy and composite restorations (Figures 5 to 8). Care was taken to re-build the collar of attached gingiva around the tooth to avoid future periodontal problems.

Figure 5. Final appearance after treatment. One composite restoration is clearly visible.

Figure 6. Rostral view after treatment.
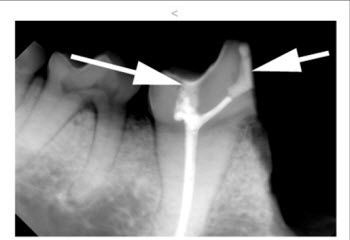
Figure 7. Final radiograph, showing the two composite restorations (arrows) and the filling in the root canal system.

Figure 8. Final radiograph, showing the root canal completely filled to the apex of the root.
The excised segment was submitted to the lab for analysis and the biopsy report confirmed the recurrence of the original tumor with appropriate margins. Re-check 60 days after surgery showed complete healing and the owner reported that the patient was able to chew hard food and biscuits on the side that was treated.
The large lower first molar (carnassial tooth) in dogs is an important chewing tooth, occluding with the upper fourth premolar to provide complete mastication. If this tooth is removed, patients frequently shift the burden of chewing to the contralateral side of their mouth, which increases plaque accumulation on the side where the tooth was removed, predisposing them periodontal disease. Extraction of the lower first molar is relatively traumatic, can weaken the mandible, and risks extraction complications that may include in mandibular fracture, damage to the mandibular neurovascular bundle and possible root displacement into the mandibular canal.
For the above reasons, treatment of this tooth is preferable to extraction whenever possible. In this case, the chewing function of this tooth was maintained by preserving most of the crown and treating the remaining portion of the tooth with root canal therapy and composite restorations. The large size of the roots of this tooth are capable of supporting the function of the remaining crown with a single root.
One point that this case illustrates is the need for biopsy and dental radiographs to guide treatment. Had the lesion been biopsied and radiographed the first time it was de-bulked, one of the anesthetic episodes would have been avoided. Additionally, had the tumor been shown to be malignant, appropriate treatment might have been pursued in a more timely fashion. Any gingival/oral mass that is removed should be biopsied. I generally treat all similar gingival lesions with conservative removal and de-bulking. Many of these lesions are the non-ossifying variant of POF’s, and conservative removal as initially performed above is usually curative.
